As a clinical pharmacist with a specialism in medicines safety, I am keen to increase the use of Human Factors and Ergonomics within healthcare. I have a strong interest in taking a systems approach to improving patient safety.
Major project
Using a Human Factors approach to explore the current opioid prescribing processes in general practices and identify facilitators or barriers to appropriate opioid prescribing.
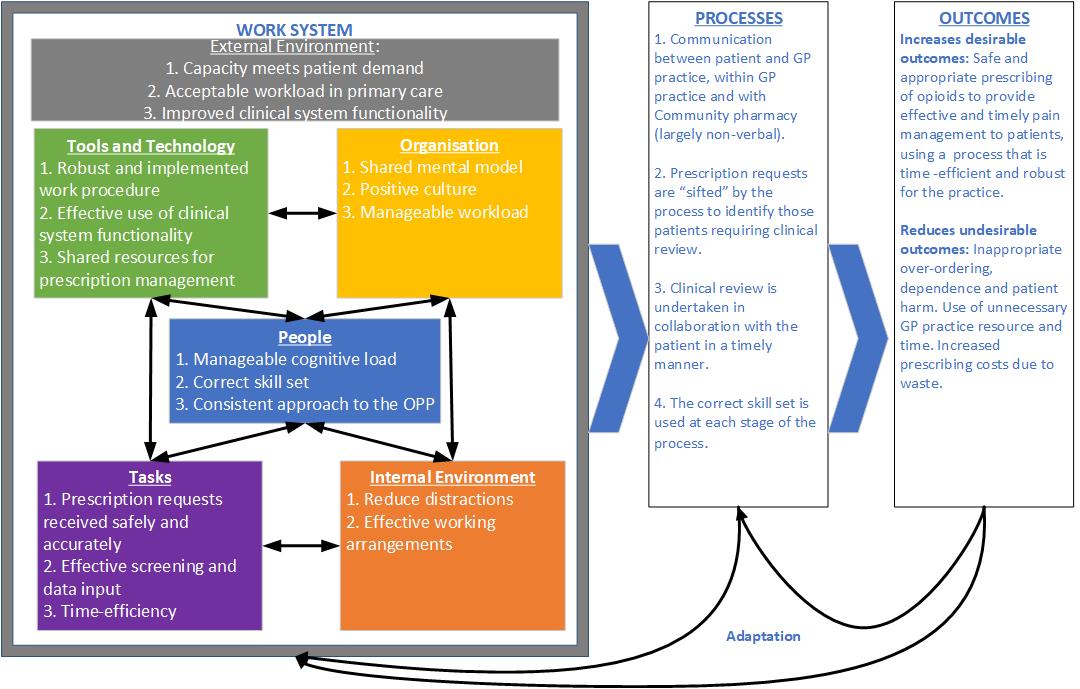
Main aims for a safe opioid prescribing process (using SEIPS v2.0)
Background:
Opioids e.g. morphine and codeine, are a group of high-risk medications that are frequently prescribed in general practices but can cause dependence and severe harm. Their use in chronic non-cancer pain (CNCP) does not have an established evidence base and is potentially inappropriate.
General practices are complex socio-technical systems that function as a subsystem of, and interact frequently with, the wider healthcare system.
Aim:
This study used a Human Factors and Ergonomics (HFE) approach to identify the facilitators and barriers for a safe opioid prescribing process for CNCP in general practice.
Methods:
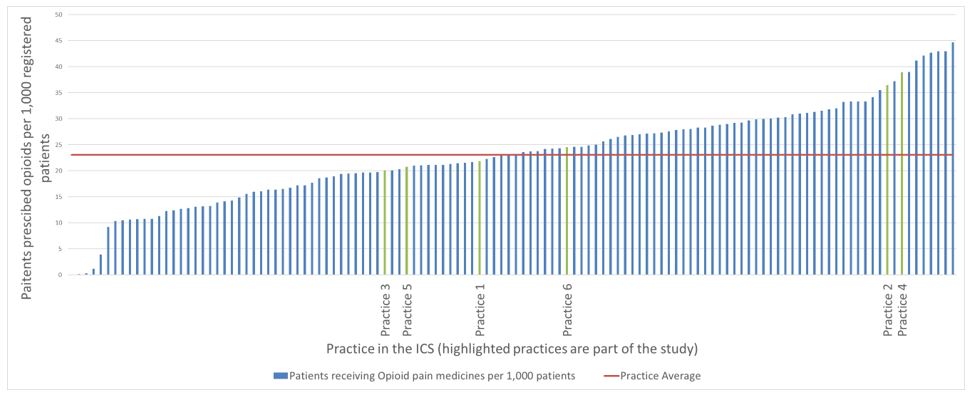
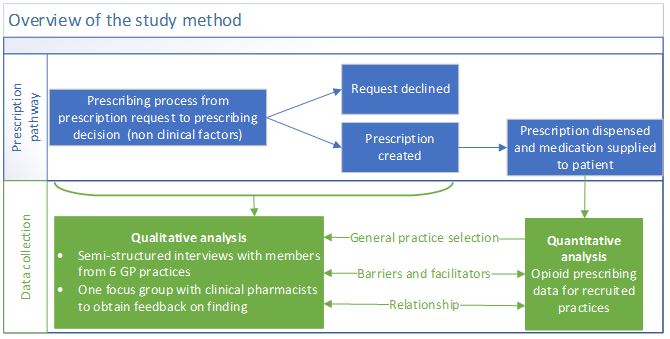
Prescribing data from the NHS Business Services Authority (NHSBSA) was analysed to facilitate recruitment and to explore a link between the opioid prescribing process (OPP) and prescribing levels.
Six general practices were recruited from 4 Primary Care Networks (PCN) within one Integrated Care System (ICS) in the East Midlands region in England.
17 semi-structured interviews were undertaken with up to three practice staff (clinical pharmacist, general practitioner, and administration roles) per practice to understand the current opioid prescribing process (OPP).
Template analysis was used to create both an expected process map and process maps for each practice. The Systems Engineering Initiative for Patient Safety (SEIPS) v2.0 framework supported the overall analysis of the process including identifying the main aims within the work system to support a safe OPP.
Interviews were transcribed and qualitative analysis performed using NVIVO 12®
The validity of the findings was explored at a small focus group (n=6).
Aims and associated facilitators and barriers for a safe opioid prescribing process.
Analysis at practice level showed that variation in the OPP was high between and within practices. It relied heavily on the clinical system whose functionality could be enhanced to better support opioid prescribing. Other improvement opportunities identified included written work procedures, clarity on roles and responsibilities, the work environment, and workload evaluation. One process would not fit all practices.
The Analysis of the OPPs for each practice using SEIPS v2.O was effective at identifying the overall aims and associated facilitators and barriers for a safe OPP. Whilst many of these are generic to all prescription processes they become crucial for opioids.
A safe OPP ensures the right patients are identified for further clinical review at the correct times. The effective use of both technology and communication is critical.
Continuing to use HFE techniques to incorporate these results into each individual practice process will optimise system efficiency and staff well-being as well as improving patient safety.
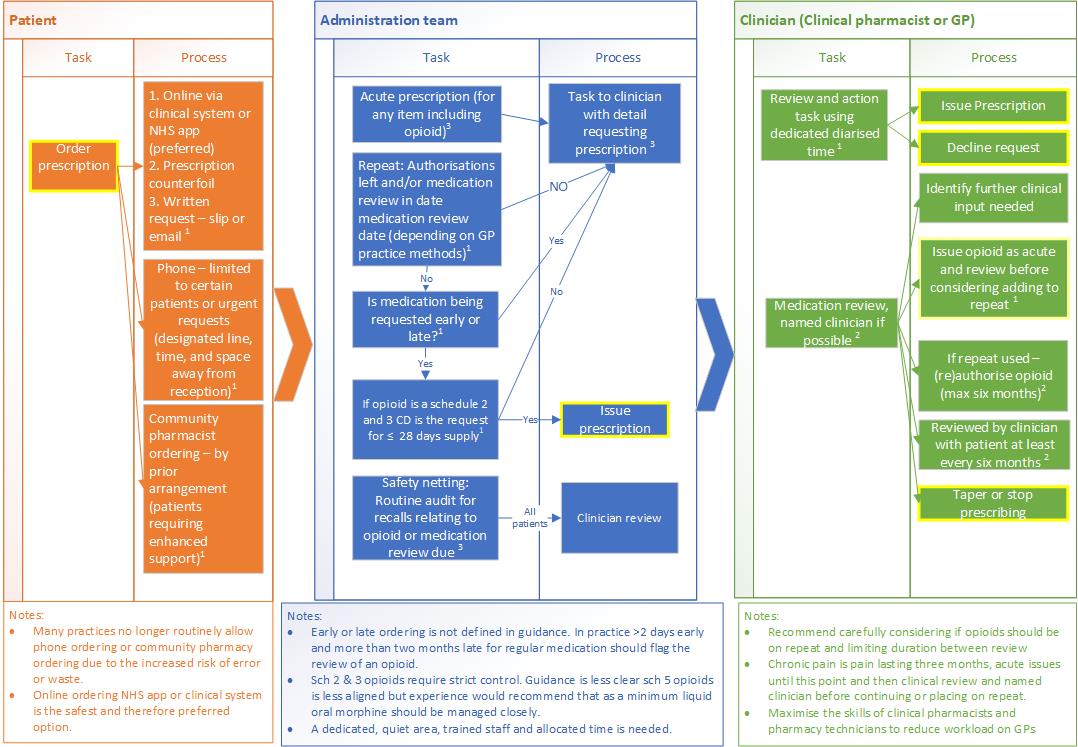
The expected opioid prescribing process used to support template analysis
Template analysis was used to create an expected OPP that covered the main practice roles plus organisational elements. This was developed using both national (albeit sparse) and local guidance, and the author's clinical experience as a pharmacist.
Interview transcripts alongside any written procedures provided, were triangulated to report the individual practice's OPP based on the expected template and identify barriers and facilitators to the process.
Whilst all practices identified opioids as high-risk medication the level of variation from the expected process was high, as was the variation between practices. Of particular note was the level of complexity in the process, how overdue reviews and early-ordering were managed, the work expected of non-clinicians, and how aligned the OPP was to non-opioid prescribing.
All practices described difficulty meeting the demands for prescriptions within the available capacity.
Integrated Care System data showing prescribed opioids per practice per 1,000 registered patients. (NHSBSA,OP1,21.6.2022-18.7.2022)
The high levels of variation in both prescribing levels and OPP across the practices is consistent with the published evidence. This variation is partly explained by the established links between prescribing levels and both geographic location and deprivation.
Whilst all practices agreed that a robust OPP supported safe opioid prescribing, no clear link could be made in this study between the OPP and opioid prescribing levels. This was possibly due to gaps in the observed OPPs and known factors having a stronger influence.
Conclusion
Each general practice is a unique complex system supporting healthcare for 1000s of patients, so effective prioritisation is crucial. Managing prescription requests is a complex process but as the risks are high with opioids, this should be reflected in the process used.
HFE was an effective approach to identify the overall aims and associated facilitators and barriers for a safe OPP in general practice. Further research to validate and evaluate the effect of implementing this study would be useful including the effect on prescribing levels and staff workload. This study supports the wider use of HFE in both primary care and wider healthcare.
Gill Gookey
Major project
Using a Human Factors approach to explore the current opioid prescribing processes in general practices and identify facilitators or barriers to appropriate opioid prescribing.